The practice of Hadi Zambarakji
The practice of Hadi Zambarakji

Guide to Epiretinal Membranes
What is an epiretinal membrane?
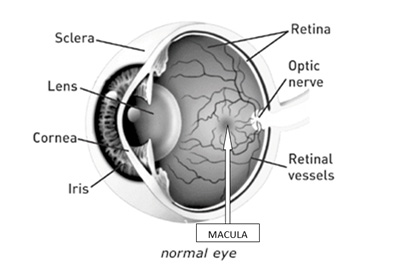
An epiretinal membrane (ERM) is a very fine tissue scar on the surface of the retina, which can contract leading to wrinkling and distortion of the retina with subsequent detrimental effects on vision. ERMs affect the vision because they may affect the macula, the central part of the retina, which is very important for fine, detailed vision such as reading.
What is the cause of ERMs?
Most ERMs result from separation of the vitreous jelly (or humour) from the retina, which normally occurs around the age of 50-60 years. This separation liberates cells, which move on to the surface of the retina where they can contract and affect the retina. ERMs may also result from other eye diseases such as inflammation (uveitis), diabetes, and retinal detachment.
What treatment is available?
The only treatment currently available is surgery to remove the vitreous (this is called a vitrectomy), which fills about 80 % of the space within the eye and to peel the membrane from the surface of the retina (membrane peeling).
What are the symptoms of ERMs?
The three major symptoms of ERMs are:
- Blurring of vision.
- Distortion – where straight edges and objects become bent.
- Ghosting of images, which may be experienced as double vision in one eye.
ERMs may be detected as an incidental finding in an eye with normal vision and no symptoms, and in these circumstances treatment is not usually required.
Is surgery always necessary?
Surgery is only required or recommended when vision is affected, which can only be determined by the patient, and this would be measured on the visual acuity chart in clinic. If the vision is stable and sufficient for that individual’s requirements without detriment to their quality of life, then surgery is not indicated. If the vision is deteriorating or distortion is an increasing problem, then surgery can be considered. Some ERMs stop progressing after an initial period and if there is any doubt then patients can be followed up in the Retina Clinic until a decision can be made. In a substantial number of patients, the ERM is “idiopathic” and identified on routine assessment by an Optometrist. Therefore several patients who have good vision and an epiretinal membrane do not need to have surgery.
What are the risks from surgery?
The most significant risk of vitrectomy is causing a retinal detachment. The chance of this happening is about 1-2%, compared with 1:10,000 risk of retinal detachment per year in the normal population. Retinal detachments can be successfully treated but the vision may be permanently damaged if the macula (the central retina) is involved. Other risks include infection inside the eye (endophtalmitis) and severe haemorrhage, both of which are uncommon (<1:1000) but can lead to severe and permanent loss of sight in that eye. Vitrectomy is also associated with an increased risk of developing cataract or worsening of any already coexisting cataract, therefore phaco cataract surgery is often performed at the same time as vitrectomy and membrane peel in patients with an early or established cataract. I would generally often recommend phaco cataract surgery to be combine with vitrectomy and membrane peel in patients over the age of 50 years.
How is surgery performed?
Vitrectomy and membrane peeling is usually undertaken under local anaesthesia as a day case. I currently routinely perform surgery using small gauge instruments (23 gauge) for epiretinal membrane surgery (see 23 gauge vitrectomy surgery handout). The operation takes about 50-60 minutes, and is painless other than the brief discomfort of the local anaesthetic injection. Some patients can still see during the operation, but this is not alarming or unpleasant, and most patients have found it a revelation. One of the major changes in the surgical technique has been the development of small gauge instruments therefore surgery can be performed through small keyholes which usually but not always do not need to be sutured (see guide on 23 gauge vitrectomy). The main advantage of this surgical approach is increased patient comfort, less post-operative inflammation and faster visual recovery.
In approximately 10-15% of patients, additional pathology is identified at the time of vitrectomy surgery, which would require laser or cryptherapy at the time of surgery, as well as the use of a gas bubble in the eye. If a gas bubble is used, the vision will be quite blurred for approximately 3 weeks until the gas bubble reabsorbs. This is usually not a concern and does not affect the final visual outcome.
What should I expect from surgery?
The primary goal of surgery is to reduce visual distortion and improve the vision. Any visual gain however, is usually small (compared to improvements in vision observed following cataract surgery). On average, 70% of patients experience an improvement of 2 lines of vision on the visual acuity testing chart and ERM surgery generally improves patients’ perception of visual function as measured using visual function questionnaires.
I have also a cataract
Many patients with ERM also have the beginnings (or more) of a cataract in the same eye. Combined retinal and cataract surgery can easily be combined if it is thought to be beneficial to the particular individual. This can still be done under local anaesthetic, and only prolongs the procedure by about 15 minutes.
Will I always need to attend a Retina Clinic?
If an ERM is stable and not progressing, most patients will be discharged from regular review, with occasional visits to their optician. If surgery is performed, patients are usually discharged about 6-9 months after the operation.
Is my vision likely to deteriorate in the future?
Unfortunately, surgery is not a cure for the effects of time on the eye and the retina in particular. Although ERMs may occasionally re-proliferate, there are a number of other ocular conditions that are more common with increasing age, including cataract (for which effective treatment is available) and age-related macular degeneration (ARMD), (please see separate guides to ARMD).
Will glasses help?
Not usually. The eye is like a camera with a lens system (the lens and cornea) and a film (the retina). If the lens system is clean (no scars or cataract) and glasses have already been prescribed or checked by your optician or optometrist, then a change of glasses is rarely of much help. Retinal surgery does not usually change the glasses prescription much, but new glasses will be needed if cataract surgery is also performed. I would usually recommend that you see your Optometrist 3 months after vitrectomy surgery for a repeat eye test and a new prescription.
Prepared by Mr. H.J. Zambarakji FRCOphth, D.M
Consultant Ophthalmic surgeon
Search the RetinaCare website
Visual guides
 Vitreomacular traction and small macular hole successfully treated with intravitreal Ocriplasmin
Vitreomacular traction and small macular hole successfully treated with intravitreal Ocriplasmin
 Macular hole (pre and post op)
Macular hole (pre and post op)
 Epiretinal membrane (pre and post op)
Epiretinal membrane (pre and post op)
 Diabetic retinopathy (medical management and laser photocoagulation)
Diabetic retinopathy (medical management and laser photocoagulation)
 Traction diabetic retinal detachment (pre and post op)
Traction diabetic retinal detachment (pre and post op)
READ HADI’S LATEST NEWS